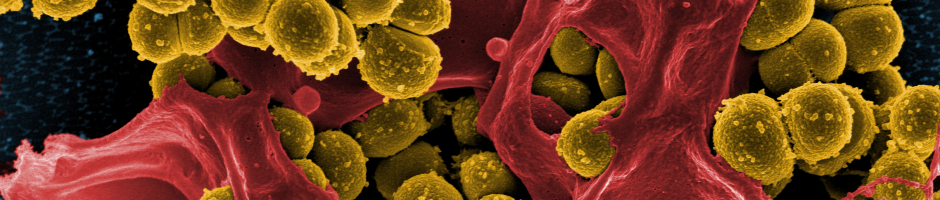
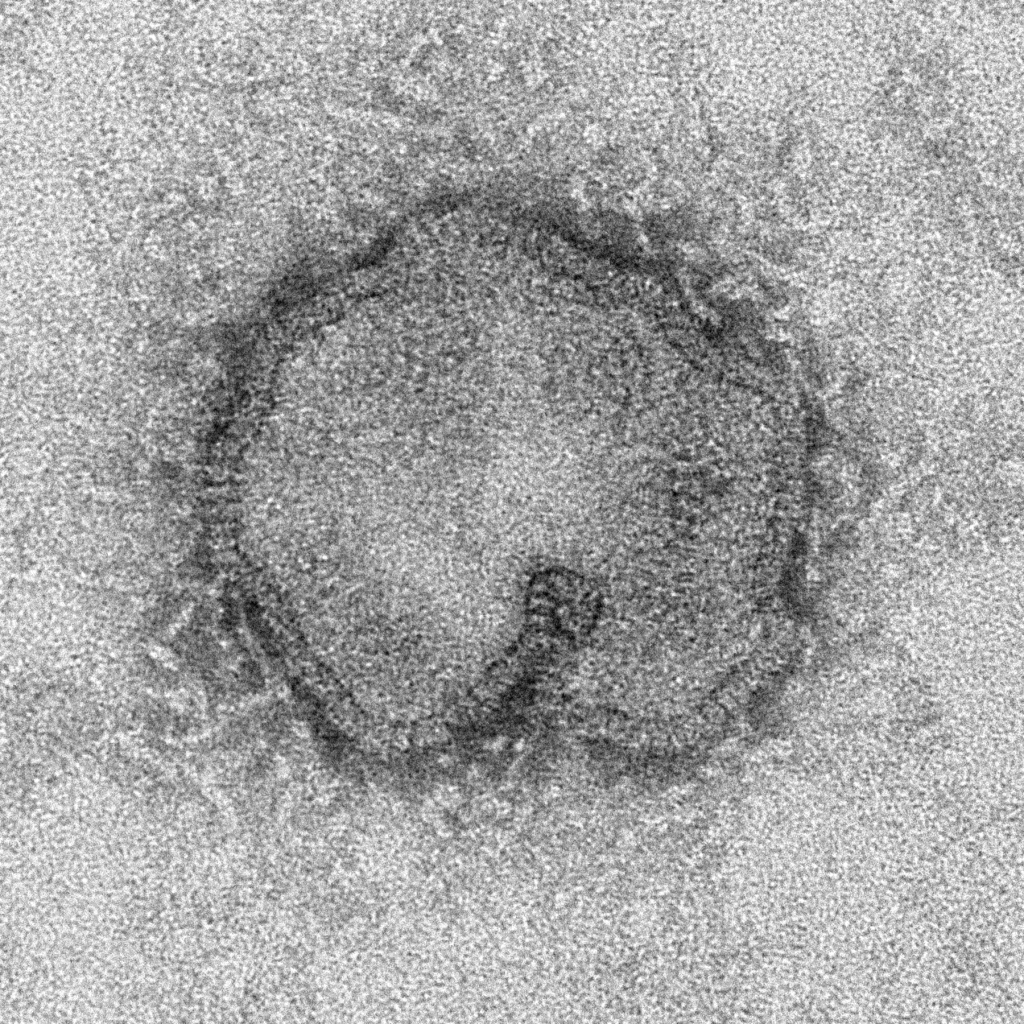
Self-awareness is fundamental to life. An organism’s awareness of itself, be it a complex multicellular animal, or a single-celled bacterium, is crucial for its ability to recognize and defend itself from intruders. Bacteria chop up DNA from invading viruses; plants interfere with an infecting organism’s ability to express its genes; and vertebrates, like humans, have a highly sophisticated immune system with diverse organs, cells, and an armament of proteins dedicated to protecting us from infection by bacteria and viruses.
Paradoxically, however, “infection,” is not only inevitable, it is a fundamental feature of our physiology. Our bodies are colonized by about 100 trillion bacteria — the commensal microbiota — that look very different from our own cells and yet are not targeted by the immune system. How these “good” microbes are spared while the “bad” bacteria that make us sick are attacked is one of the biggest questions in immunology today, causing many to rethink what they thought they knew about immunity.
Our immune system uses pattern recognition to identify foreignness. Pattern recognition takes advantage of the long evolutionary distance that separates humans from microbes like bacteria and viruses. Because we’ve been evolving separately from these organisms for billions of years, there’s a lot about them that looks different from us, even on a single-cell level. Bacteria have unique sugars on their cell surface, they use specialized molecular motors for movement, and their genetic material is structurally distinct from ours. Because these differences are present in all bacteria but entirely absent from human cells, recognizing these pathogen associated molecular patterns, or PAMPs, is a highly efficient way for our immune systems to detect potential threats.
This immune pattern recognition evolved long before humans did. Plants and invertebrate animals such as fruit flies also use pattern recognition to identify foreign invaders that may cause disease, in a way that is remarkably similar to humans. All organisms that employ this strategy use specialized molecules called pattern recognition receptors (PRRs), each of which specifically detects a particular microbial PAMP. These PRRs are expressed on various cells of the immune system and at barriers between our bodies and the outside environment, allowing for rapid recognition and elimination of invading microbes.
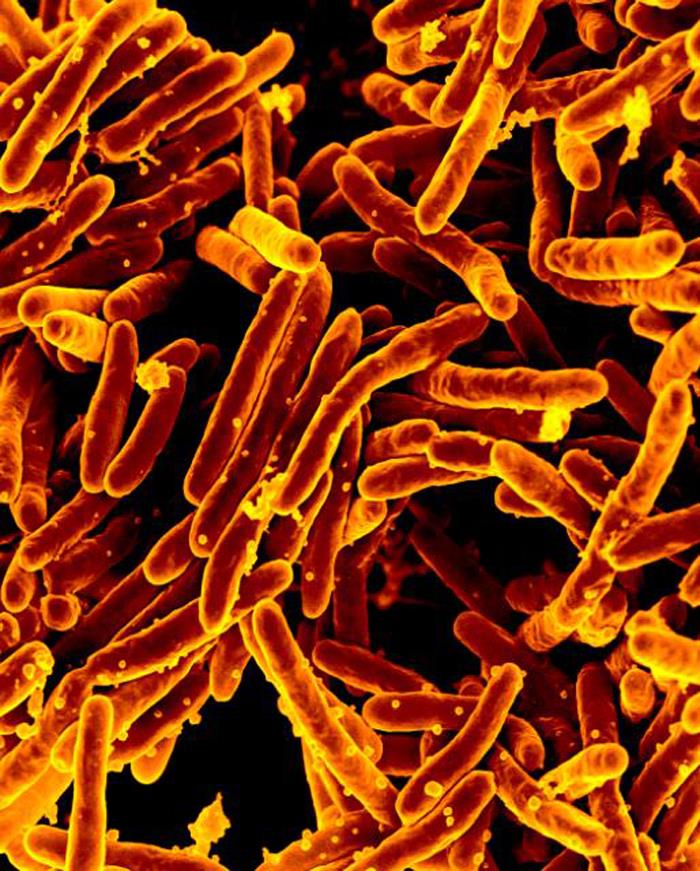
PAMPs are part of all bacteria, from the deadly Mycobacterium tuberculosis to the beneficial Bacteroides thetaiotaomicron that thrives in the human gut. Not all bacteria are harmful invaders: the microbes that live in our bodies are increasingly being recognized as being fundamental to life, another “organ” as necessary as the heart, liver, or kidneys. Our microbiota break down complex nutrients, synthesize essential vitamins, and help prevent infection by pathogens that cause disease. They even facilitate the development of our immune system itself — without a commensal species called segmented filamentous bacteria, we fail to develop certain types of immune cells essential for fighting infections with pathogenic bacteria. Comparing the numbers of human to microbial cells in the body, it would appear that we are far more bacterial than human, and yet the immune system’s strategy of pattern recognition seems to render our microbiota guilty by association. How do these 100 trillion bacteria persist in the presence of an immune system that is specialized to seek and destroy them?
There are a few hypotheses to explain this apparent paradox. The first, and simplest, is compartmentalization. The surface of the gut, which is where the vast majority of commensal microbes reside, is covered in a thick layer of mucus that protects lots of these microbes from the immune system. Trapped in the cozy mucus layer they aren’t recognized at all so there’s no need to distinguish them from pathogens. However, this can’t be the full story, as we know that some of our gut commensals traverse this mucus layer, and that some of our immune cells can extend arms into the mucus layer to search for pathogens. Sometimes they encounter pathogens, but most of the time they encounter commensals, with no apparent consequences.
Perhaps instead of the microbes being able to hide, the explanation is that our immune system is able to distinguish between good and bad microbes. If this is the case, scientists haven’t found out how the immune system might do this yet, though there are a number of fascinating hypotheses. Different species of microbes are specialized for breaking down different types of food in the gut, and it’s possible that the distinct metabolic byproducts of commensals and pathogens could be recognized as a proxy for their relative abundance. Similarly, pathogens and commensals tend to behave differently from one another, and the immune system may recognize certain features of pathogen “bad behavior,” such as the expression of toxins that kill our own cells. Though these hypotheses stand to be expanded upon, what remains entirely unclear is how our body recognizes and controls so-called “pathobionts,” bacteria that are helpful the vast majority of the time, but occasionally exhibit naughty, pathogen-like behavior. Might our immune systems recognize otherwise helpful bacteria that have decided to, for example, feast on the mucus molecules in the gut? We know that some of our commensal bacteria do this, but whether our immune systems recognize it as problematic is unknown.
But maybe it isn’t our immune systems that are smart enough to distinguish between which bacteria belong and which don’t. Maybe it’s the microbes that are outsmarting our immune systems. Perhaps the good microbes, those that have evolved to treat our bodies as a specialized habitat, have also devised ways of hiding from our immune systems. All organisms evolve to deal with the positive and negative aspects of their habitats, and bacteria are no different. A recent study in Science showed that, unlike pathogens, certain commensals tend to be more resistant to antimicrobial peptides (AMPs), molecules secreted by our gut immune cells that are intended to kill bacteria. While it was previously thought that all bacteria were equally susceptible to AMPs, this study showed that an intestinal pathogen, Clostridium dificile, was susceptible, while a commensal, Bacteroides thetaiotaomicron was resistant. The commensal’s AMP resistance allowed it to remain alive while the immune system deployed AMPs to destroy the pathogen, indicating that microbial resilience may be an important solution to the paradox of the spared microbiota.
The explosion of research about the microbiota thus far has largely focused on how our commensal bacteria impact our health. As the list of helpful functions that our commensal microbiota perform continues to grow, the mystery of their resilience in the face of the formidable mammalian immune system becomes ever more perplexing. Not only does this question have important implications for how immunologists conceptualize self and non-self, it could also be a key component in the understanding of diseases that seem to be driven by aberrant immune responses to good bacteria. To the extent that our commensal bacteria are part of our identity, our immunological self-awareness will increasingly be understood as encompassing our microbial and non-microbial selves.